More than a year following passage of Medicaid expansion by a ballot measure, a Cole County Circuit Court judge issued a final order on August 11 in the litigation seeking to advance Medicaid expansion, directing the state to proceed with implementation of expansion immediately. The ruling follows a unanimous ruling by the Missouri Supreme Court that upheld the constitutionality of Medicaid expansion.
This now clears the way for thousands of eligible low-income and uninsured Missourians to secure health coverage through MO HealthNet, the state’s Medicaid program.
Prior to Medicaid expansion, Missouri had some of the strictest eligibility criteria in the U.S. Adults who are not parents could not qualify for Medicaid, regardless of how poor. A non-disabled adult with children qualified for coverage if their income was below 21 percent of the federal poverty level. That meant a family of four must earn less than $5,550 a year. Among those who fell into the coverage gap, 75 percent were childless adults and 63 percent in a household with at least one worker. Among those who currently sit in the coverage gap, 75 percent are childless adults and 63 percent are in a household with at least one worker. Now, those income eligibility criteria have been expanded to 138 percent of the federal poverty level. For a single person in 2021, that means the highest income a person can earn and still get coverage is $17,774; for a family of four, the income limit is now $36,570.
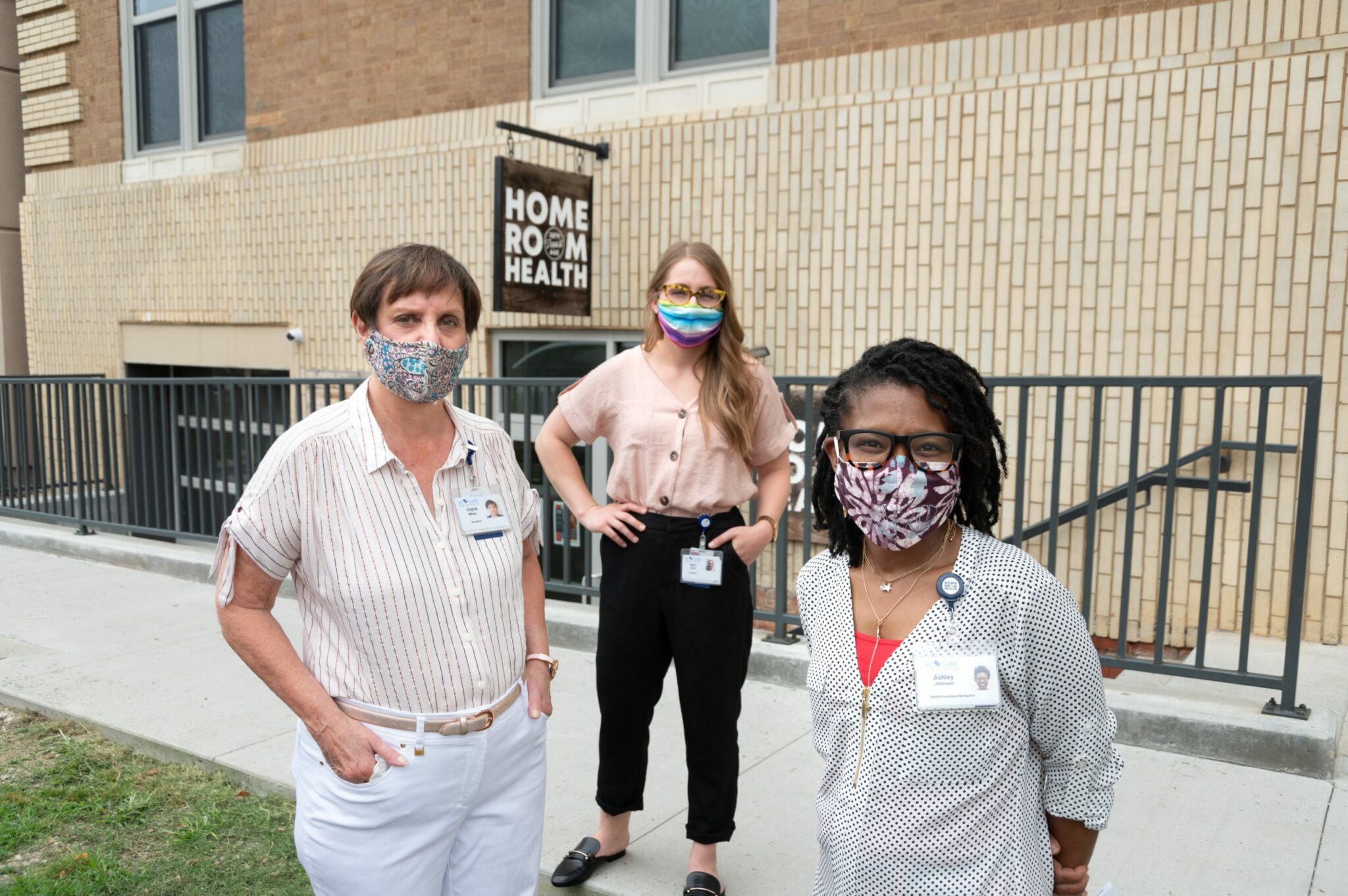
Brenda Sharpe, REACH President and CEO, said the latest ruling places a priority on educating the public on this new coverage opportunity.
“Although we celebrate this ruling, the work of health care organizations, advocates and other groups continues. We will need to work swiftly to educate the public about MO HealthNet and the health and household financial benefits of coverage. The REACH Foundation will do our part to aid implementation by continuing investments in health partners that provide quality enrollment assistance.”
Sharpe said the foundation will work with health partners to identify ways to strengthen outreach and enrollment to help Missourians take full advantage of the expanded coverage.
As a strategy in the foundation’s Enroll All Eligible outcome area, REACH has funded the work of qualified health navigators and enrollment assisters to help people understand their coverage options and enroll. In 2020, REACH awarded enrollment assister grants totaling $300,000 to increase enrollment for health coverage and other public benefits; total investments in this area is $1.94 million since 2016.